#319 New CPT Code 96041 Explained: 2025 Billing for Genetic Counselors
DNA Today: A Genetics Podcast
Deep Dive
Why was the new CPT Code 96041 introduced for genetic counselors in 2025?
The new CPT Code 96041 was introduced to address the outdated 'face-to-face' language in the previous code, making it more inclusive of telehealth and recognizing the total time genetic counselors spend on patient care, including preparation and documentation. This change aims to improve billing accuracy and reimbursement for genetic counselors.
What are the key differences between the old CPT Code 96040 and the new CPT Code 96041?
The key differences include the removal of 'face-to-face' language, allowing for total time billing, and the inclusion of non-face-to-face activities such as preparation and documentation. This change better reflects the comprehensive work genetic counselors do and ensures more accurate billing.
How does the new CPT Code 96041 impact documentation and billing for genetic counselors?
The new code requires genetic counselors to document the total time spent on patient care, including preparation, counseling, and follow-up. Institutions are creating standardized language and tools to help counselors accurately report this time, ensuring compliance with billing requirements.
What activities are now eligible for billing under CPT Code 96041?
Activities eligible for billing under CPT Code 96041 include preparation, counseling sessions, documentation, and follow-up communications. This comprehensive approach ensures that all time spent on patient care is reportable.
How does the new CPT Code 96041 broaden access to genetic counseling services?
The new code supports telehealth, making genetic counseling more accessible to patients regardless of their location. It also allows for more accurate billing, which can lead to better reimbursement and more widespread availability of genetic counseling services.
What is the 50% rule, and does it apply to CPT Code 96041?
The 50% rule, which applies to evaluation and management codes, requires that at least half of the time spent on a service must be face-to-face with the patient. However, this rule does not apply to CPT Code 96041, allowing genetic counselors to bill for any combination of preparation, counseling, and documentation time.
What are the potential hurdles in payer reimbursement for CPT Code 96041, and how can they be addressed?
Potential hurdles include payer contracting and credentialing, especially in states without genetic counselor licensure. Genetic counselors can address these by working with their institutions to develop internal processes and by advocating for recognition and credentialing with payers.
How does the new CPT Code 96041 impact billing for genetic counseling assistants (GCAs)?
GCAs are valued as part of the code, but their time is not reported separately. It is assumed that their tasks are part of the standard care process and are included in the total time reported by the genetic counselor.
What is the role of the National Society of Genetic Counselors (NSGC) in educating stakeholders about the new CPT Code 96041?
The NSGC is providing resources and education to help genetic counselors and institutions understand and implement the new code. This includes webinars, presentations, and a dedicated webpage with FAQs and clinical workflow considerations.
What is the significance of the Access to Genetic Counselor Services Act in relation to CPT Code 96041?
The Access to Genetic Counselor Services Act is crucial for getting genetic counselors recognized as independent providers by Medicare. This recognition would improve reimbursement and encourage private insurance companies to follow suit, enhancing access to genetic counseling services.
- New CPT code 96041 effective January 1st, 2025
- Shift from "face-to-face" to "total time" billing
- Includes prep time, patient time, and documentation time
- Telehealth eligible
- Addresses the need for updated billing practices to reflect genetic counselor's activities
Shownotes Transcript
Looking to jumpstart your career as a genetic assistant? These essential roles involve patient communication, data management, genetic testing coordination, and admin tasks, making proper training a must. The Genetic Assistant Online Training Program at Johns Hopkins University School of Medicine is a top choice. DNA Today listeners rave about how this course boosted their genetic counseling skills and prepared them for grad school.
The spring cohort starts soon on January 27th, so apply now before it's too late. The program includes two 10-week instructor-led courses. Armed with a basic science background, you'll earn a certificate from the Johns Hopkins School of Medicine upon completion. You'll also gain practical skills and insights from leading instructors that will give you a competitive edge in genetic counseling and related fields.
Learn more at dnapodcast.com slash sponsors or simply search Genetic Assistant Online Training Program Johns Hopkins.
When it comes to your health, knowledge is power. I've always believed that the more we understand about our bodies, the better decisions we can make, whether it's about the food we eat, the exercise we choose, or how we plan for the future. But traditional healthcare often feels reactive and not proactive. That's why I'm so excited about 23andMe Plus Total Health, a longevity platform that puts you in the driver's seat of your health journey.
With 23andMe plus Total Health, you get advanced genetic screening, giving you insights into your potential future risks, and comprehensive blood testing throughout the year to track how your health is changing. It's a level of personalized care that goes far beyond the one-size-fits-all healthcare system that unfortunately we're used to. Advocate for your health today. Go to 23andMe.com slash DNA Today to receive 10% off your Total Health membership.
Again, that's 23andMe.com slash DNA Today. You can also find this link at DNAToday.com. Take charge of your future health with 23andMe Plus Total Health because your health deserves a personalized approach. How is it that we find ourselves surrounded by such complexity, such elegance? The genes of you and me. The genes of you.
They're all made of DNA We're all made of the same chemical DNA
Hi, you're listening to DNA Today, a multi-award winning podcast and radio show where we discover new advances in the world of genetics. From genetic technology like CRISPR to rare diseases to new research. For over a decade, DNA Today has brought you the voices of leaders in genetics in over 200 episodes. For the past three years, DNA Today has won the People's Choice Best Science and Medicine Podcast Award. I'm Kira Dineen. I'm a certified genetic counselor and your host. ♪
With 2025 right around the corner, we're discussing the brand new CPT code 96041 that will be effective January 1st. So very timely right now to be talking about this. It's going to be a game changer for the genetic counseling profession. And lucky for us, we have two experts to break this down for us. I've watched them speak about this multiple times, but I still have a lot of questions and just want to make sure I'm understanding things right.
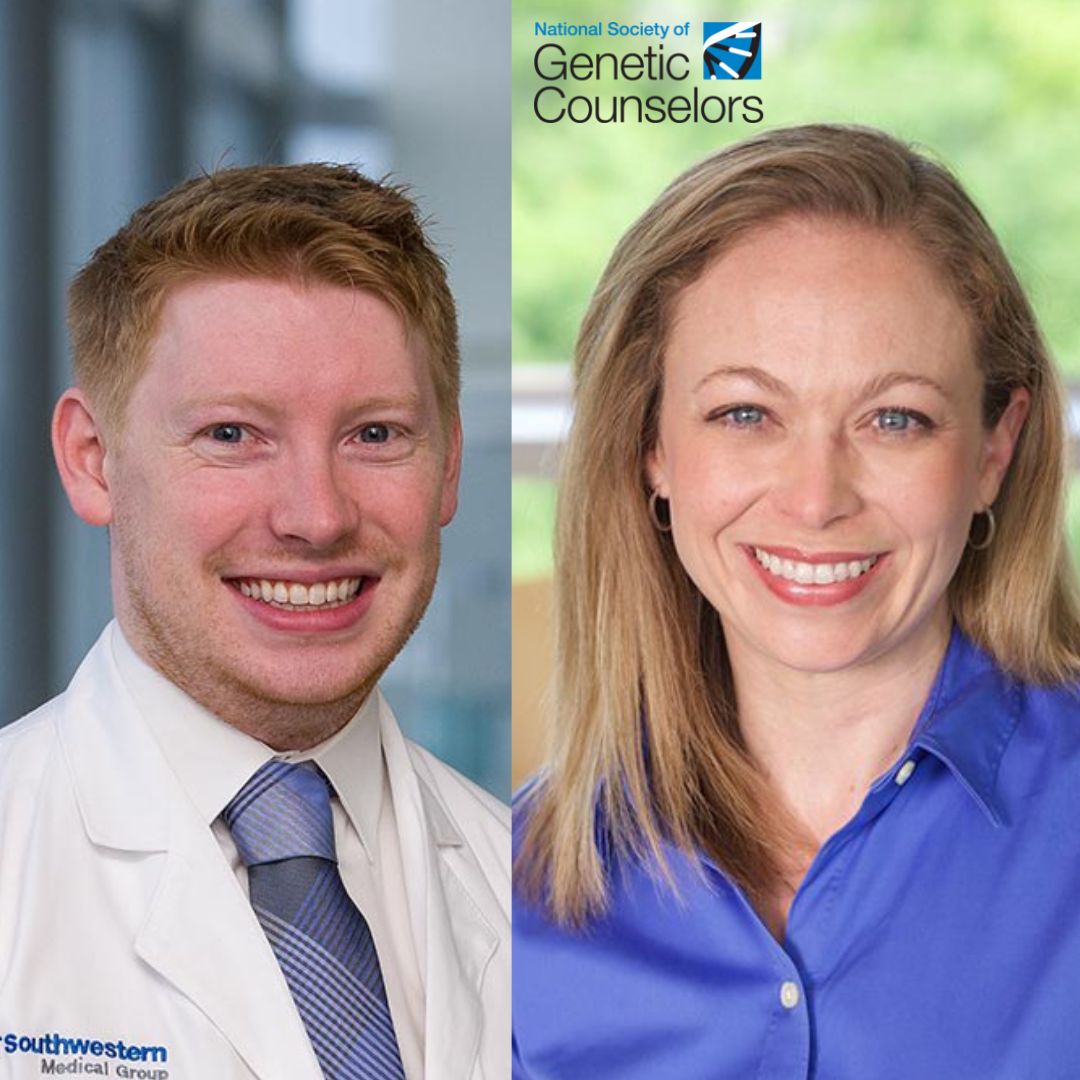
So we have Dr. Colleen Campbell, who is in her last weeks of her NSGC presidency. She also holds the title of Director of Genetic Counseling Operations for University of Iowa Health Care. We're also joined by Ryan Reyes, who I realize we started these conversations years ago. And you're like, we'll circle back about a new code.
Brian is a cancer genetic counselor and manager at UT Southwestern's Cancer Genetics Program. He also serves as a CPT coding advisor to NSGC. So I want to get into how this new code affects billing and what genetic counselors need to know to
Before it is active January 1st. So who wants to start us out in explaining the significance of this new CPT code? It's one number different from the old one. 041. How it differs from that old one. Aline, I don't know if you felt the same way I did when we found out that the number was only one higher. But that was a surprise for us. Because we didn't know at the conference, right? At the conference, we didn't know what the code would be.
We found out days before and Colleen and I had been like, what is this number? What is this number? And they were so kind to give us permission to release before the book even came out, the American Medical Association. But we were really excited because this has been years in the making and something that
We've been really excited about the code needed a refresh to make sure that is up to date with other codes and really address the needs of that face to face language that was confusing people about. Yeah. And that's a big part that the pandemic, I think, also pushed in terms of a lot more counselors doing telehealth. I am now fully telehealth or like, you know, just in 2024.
That happened for me. So what was the need to update this code? Why was it necessary in the field? What is different from the original code? I think the big thing that genetic counselors will notice is that face-to-face language is gone. And we're really excited about that because there was confusion.
When it said face-to-face, people thought that can't mean telephone, but it had always meant that it was telehealth eligible, but it was just confusing language. And we were really excited to see that when the AMA updated that for us, they actually did so for all of the codes that used similar language at the same time.
We also really wanted to recognize that genetic counselors are doing more than just spending time face-to-face with patients. We prep to see our patients. We put pedigrees together. We get records to make sure that if there's genetic testing that's been done in the family, we know about it ahead of time and can have an informed conversation with our patients.
And then we spend a lot of time documenting and making sure that the care team knows what genetic testing means. And this change is really going to help us make sure that we're capturing, documenting that time in a reportable way.
Yeah, it's so important because I'm a prenatal genetic counselor part-time. And so a lot of my time is spent going through records from maybe their OB, if we're not their OB, going through that. Okay. Oh, I met them before. Let me read through from that original pregnancy that I met them for. And then calling out the results. So all of these aspects of what we do for one patient that's not in the counseling session are really being included. I probably shouldn't say included.
all, but like a long list that you're describing.
Yeah, I think that when genetic counselors think about what they can report and document with this new code, we can really lean on our colleagues that use the evaluation management code. So our colleagues that are physicians and APPs. Colleen and I both work in practices that are trying to integrate this new code. Colleen, what's your group doing when you're thinking about how you're going to document these services? For the genetic...
how the genetic counselors are going to document. So actually, our billing team is creating language that they're going to just have the genetic counselors drop in. It'll be a smart phrase, and they'll just document the amount of time that they spent with prep and total time day of service on the case, which will include not only the time with the patient, but that prep and follow-up time as well. So it'll be a pretty...
Simple update because right now we're already billing for the services and we already include the language for face-to-face time and how much time we spend. So it's just updating that slightly, tweaking that language. We're similar. I would say our biggest question is like, how do we measure the time? So we've had some anxiety about like calculating minutes. And so we've even explored like within our EMR.
Are there automated calculators that you can use so it can track how much time you have a patient's chart open? There's a lot of logistics to think about with that. You don't want to count time that's really not being spent in service to the patient or that's just administrative. Things like finding the correct tab is not patient care, but it's certainly something I do a lot. And we're just figuring that out together as a team, working with other practices that really do the same thing on a regular basis because their code is more recent.
Other people do this all the time and it's not just in health care, but throughout, you know, society. Right. Lawyers bill for their time. And, you know, I also am the assistant director of a genetics institute where we have bioinformaticians. They bill for their time. So there's a lot of different tools out there and it doesn't have to be perfect. We're not talking like down to the second. Right. But how do we, you know, more accurately represent our time will be helpful.
And one part that I remember learning about during one of the NSGC conferences, one of the presentations that Brian, at least you were a part of, I don't remember which ones. It's hard to keep track because you guys have presented on this multiple times because we all need to learn about this. But that
You can't prep the night before for a patient the next day and count that all together. And that's usually my flow. So usually I'm like, all right, let me look at the next day's schedule, make sure all that's prepped so that I'm like, all right, great, I've worked ahead. But I'm going to need to adjust how I do that and wake up earlier in the morning and prep for the patients that day so it can all be built together. Is that the correct way to do it?
It is. And we know, y'all, I promise that when- GCs are planners, we're organizers, this is hard. Yes, we want to do things the right way. We know that getting records ahead of time can give us more time to make sure that they're correct.
We are not saying that you need to change anything that would negatively impact patient care. If getting the records multiple days ahead of time makes sure that you get the correct records that you need the right way, then keep doing that. But if there are things that we're doing just because it's convenient for us or just because our type A personality genetic counselor feelings are like, oh, but I want to do it the night before. And
and it's not directly bettering patient care, then documenting the morning of or working on those things the morning of is what everyone else in the medical field is also having to do. And so these are standards that we did discuss these and that other professions would love to be able to do these things too. But when we were thinking about this, we were really thinking about
at Colleen and the board are really asking us to bring us in line and modernize us with the rest of medicine. That's where we want tonight counselors to be, right? And we can't do that while always being the exception. And so when we were having these conversations with the AMA and updating the code, we recognize that we can't always be the exception. And in this case, it wasn't an option. That wasn't something that we could do differently from everyone else. And so this is an opportunity for us to really capture things that
that weren't even being captured before. So we see it as a huge win. It's not going to work for everyone, but I certainly think that there's ways to adapt and make it work for you.
It would just add to that, you know, when we think about job security, too, it's important for employers to be able to recognize what you spend your time doing. And with the old code, we weren't able to accurately do that, right? And they only saw like maybe what half your time was spent doing. So when you want to hire another genetic counselor or grow your team, it's
It's important to be able to show like how you're spending your time. And that's both in the documentation and also those calling out of results and things like that. And that's what's really exciting about the new code is it should help with that. And I think to Brian's question earlier about like, what are we doing differently? Honestly, like our biggest conversations are more about schedule templates, real estate, clientele.
Clinic space is tight, right? And if all of a sudden you're going to change your template to better capture your reimbursement for your time, you're going to need to like coordinate that. And so those are the conversations that we've been more focused on our scheduling and where our rooms are going to be and things like that, because the code itself, since we're an institution that already built, the code itself will flip over.
I'm going to be making more money because we weren't billing for all of this other prep time or results time, all this other direct patient care time that we're spending this time on Jane Doe and not just as Brian was saying, administrative stuff. Oh, let me redo some templates, stuff like that. Right. That's the admin side separate. But.
institutions that we work at are going to be getting reimbursed more, if I'm getting this right, for our time. And they're like, wow, the ROI and genetic counselors have really improved. And one thing that I think a lot of people
knew about, but to hear the statistic from you, Colleen, is it the presidential address? Am I getting that right? Where you addressed everybody at NSGC that the May 2024 graduating class had about 29%-ish, if I'm remembering it right, my notes are not in front of me, scary thing,
had jobs at graduation. That has gone up. By August, that number looks much better. But that's something that I'm really concerned about in our field, that it's like, what is going on? Because genetic counselors are needed. The demand is high, but somehow there's not a lot of jobs out there. And I'm hoping that this code, along with some other things that maybe we'll touch on
will help that because then institutions see, oh, we're spending X amount on this genetic counselor's salary. And this is how much we were paid for the work they were doing by insurance companies and everything. Oh, that's great. We have this wait list of patients. Yes, let's hire another one because we see that the money is going to work out. Is that what we're hoping is going to happen with this?
Yes, exactly. This along with other things like you pointed out. So you're exactly right. There's a demand for genetic counseling. You know, the patients need it. The providers are asking for it. We have a workforce ready to go and a workforce that's rapidly growing. And that missing link is really the reimbursement and improving that reimbursement, which is why the board has focused so heavily on that.
reimbursement piece for our new strategic plan for 2025 through 2027, and really hitting on reimbursement on all fronts, because we do know that we need to meet that patient and provider demand for our services. And we want to keep growing our profession, right? That's great for everyone involved. So I think you're exactly right. We're hoping this new code that better accounts for our time will help hospitals get better reimbursed for our time and then be able to
continue to employ genetic counselors as well as hire additional genetic counselors. And with that, I'm wondering...
You both work in states that are different in terms of licensure. So Brian, I've heard you talk multiple times about how you've been able to have genetic counselors that you manage in Texas still have billing, being able to bill for their time, even though you're not in a state with licensure. And Colleen, you're in a state with licensure in Iowa. I'm also in a state with licensure. So I can, you know, it hasn't been a hard time.
thing for our office, the private practice I work at to bill for my time. There doesn't need to be a doctor associated with the visit. It's just, just me often ultrasound, whatever, but they could just be meeting with me. So I'm,
Is there any role that that plays? Is it just another hurdle, Brian, in terms of what you've experienced in Texas? Because, you know, we're not a lot of states still don't have licensure. More than not, I think. Yeah. 36 states do have licensure bills passed. Really excited because the code changing gives NSGC the perfect opportunity to rehab conversations that we had years ago with payers, but in a 2024-2025 environment. We
We can now say genetic counselors are here to stay. Yes, back when we had these conversations, many payers did recognize genetic counselors, but we know that for genetic counselors, the pain point probably isn't 96040 and probably won't be 96041. The pain point in billing for the majority of genetic counselors probably exists in the payer contracting and credentialing step.
that recognition of genetic counselors as independently billable practitioners. That's a challenge in particularly states that don't have licensure because one of the most important parts of payer contracting is credentialing, making sure that the genetic counselors are licensed and also that they're free of malpractice. That's something that states that have licensure
have a built-in state-recognized system for that states that don't have licensure don't. And so for practices like mine, we had to develop an internal process and could convince our own credentialing team to credential us and make sure that we have those things so that when we had conversations with payers, they could say, no, our genetic counselors are legitimate. We can trust them, and therefore we should contract for their services.
And if you're at a smaller institution or if you're at one that is not willing to have those conversations, it can be a real burden to move the needle in that conversation. I'm hoping that this will give Colleen and the board and NSGC the leverage to then re-have these conversations with payers to just say, now that we're in 2025, let's reopen this conversation and seal the deal.
Looking to jumpstart your career as a genetic assistant? These essential roles involve patient communication, data management, genetic testing coordination, and admin tasks, making proper training a must. The Genetic Assistant Online Training Program at Johns Hopkins University School of Medicine is a top choice. DNA Today listeners rave about how this course boosted their genetic counseling skills and prepared them for grad school.
The spring cohort starts soon on January 27th, so apply now before it's too late. The program includes two 10-week instructor-led courses. Armed with a basic science background, you'll earn a certificate from the Johns Hopkins School of Medicine upon completion. You'll also gain practical skills and insights from leading instructors that will give you a competitive edge in genetic counseling and related fields.
Learn more at dnapodcast.com slash sponsors or simply search Genetic Assistant Online Training Program Johns Hopkins.
When it comes to your health, knowledge is power. I've always believed that the more we understand about our bodies, the better decisions we can make, whether it's about the food we eat, the exercise we choose, or how we plan for the future. But traditional healthcare often feels reactive and not proactive. That's why I'm so excited about 23andMe Plus Total Health, a longevity platform that puts you in the driver's seat of your health journey.
Again,
Again, that's 23andMe.com slash DNA Today. You can also find this link at DNAToday.com. Take charge of your future health with 23andMe Plus Total Health because your health deserves a personalized approach.
Yeah. And I just want to, and Brian said this, but just to emphasize, licensure does not equal reimbursement and the credentialing. But what licensure does do is identify and give that title protection to who is a genetic counselor and how they're trained. And that's the piece that, you know, payers are looking to see, like,
Is anybody calling themselves a genetic counselor or who is defined? And so that's the part that title protection is the part that's really critical for that credentialing piece.
So it's not needed to be able to bill, but it's harder sometimes to get there in institutions and convince them, hey, we need to be doing this. And I've never worked in a billing department, but I would think if someone's coming and saying, hey, I do all of this work, you pay me a salary, let's try to get money. Shouldn't they be like, oh yeah, you're talking about us making money? Yeah, let's have this conversation, figure it out. Do you have any advice for genetic counselors going to,
the billing department or whatever that's called and saying, hey, we need to start doing this, probably a little bit easier if they've been using the old code to say, hey, we just got to update this. But then there are some that maybe aren't even billing because maybe they're thinking, well, we don't have licensure. I'm thinking like in for me, New York is 10 minutes away and New
New York's genetic counselors are not licensed. So I knew getting a job, all right, in Connecticut, I'd be licensed, New York, I wouldn't be. So I'm getting that extra letter if I live in Connecticut and work there. Is there any advice for genetic counselors that are listening to go to their bosses, or maybe they send their boss this episode, or the billing department, whoever that person is?
Yeah, I absolutely have advice. I think when we think about money and we think about billing, we often think that this is a very rigid process. I know when we started billing in 2019, that was my thought. I was like, this is going to be terrible. We're in an unlicensed state. Like the world is going to burn down around us. And what I learned is that the billing process
process in the United States is so much more flexible than you might think. A biller may prefer a particular telehealth modifier and use that over the standardized modifier that the American Medical Association recommends. That seems really odd to us as people that are as maybe as a field tend to be rather rule following. And so one of the things to recognize is that
Wholesome examples together. Find some practices in an unlicensed state or practices similar to yours and bring those as examples to your billing team to show them how it can work in a setting similar to yours because they may be thinking about billing from
one particular viewpoint, and that may not match what's actually happening in practices that are billing like yours. And how does this work in terms of, from my understanding, this new code 96041? We'll just keep saying it so that people are like, right, that's the new code. It's not currently covered by Medicare. So how does that work in terms of what needs to change in order for genetic counselors to be recognized by Medicare? Because it seems like
When that happens, a lot of private insurance companies then follow what Medicare is doing. So it feels like that would be awesome because then a lot of insurance companies are going to follow suit. What do we need to do to get there? Is that the Access to Genetic Counselors Act? Is that where that fits in? Yes, that's exactly where that fits in because you're right. A lot of payers will follow Medicare's lead.
And so we really do need to pass the Access to Genetic Counselor Services Act. And so that's where the board of directors had issued the RFP for a refreshed strategy. And like I mentioned earlier, really want to push on all fronts for reimbursement. So Medicare, commercial payers, Medicaid, and really move the needle to close that gap between the patient demand and our workforce, our growing workforce. And so with that right now, Medicare actually reimburses for genetic counseling services.
formed by recognized Medicare providers. So other providers can bill and get reimbursed by Medicare for genetic counseling. We're just not yet a recognized provider type. Which is wild that a nurse can say, I'm doing genetic counseling. This is great. All right. Awesome. I'm getting reimbursed and everything. And then for genetic counselors that specifically got a two-year master's degree in
in genetic counseling sat for our boards passed we aren't doing genetic counseling in terms of being approved by medicare exactly yeah so and it's audiologists there's a lot of a lot of provider types and so that's one of the things though that is nice is that we're not trying to add a new service to medicare which would definitely like drive up costs we're just adding a
provider type. And so other people are already billing Medicare for these services. And if we're able to bill Medicare for these services, we would bill at a lesser rate than physicians. And so we think that this won't drive up the costs for Medicare significantly. Yeah. And so I have some logistic questions because people listening, they're going to be like, all right, we're using this new code. How am I using it differently? So from my understanding, when a patient comes in,
they can only have one consult. So either myself, the nurse practitioner, or the MFM I work for, we can't all meet with that patient the same day and all bill for that service.
I don't know. That seems to be in general. It doesn't seem to be a unique thing to genetic counselors. So is that the same case with this new code that either they've got to meet with me or the MFM because if they meet with both of us, which sometimes is necessary, right? And we're like, we don't care about the billing. We just, we really need the MFM's perspective and me as the genetic counselor. And sometimes we'll do sessions together. But
But in the normal standard workflow, we want to make sure those appointments are on different days. So is that the same with this code?
So when we talk about multi-provider visits, one of the most important things, advice for anyone is you should definitely have a conversation with your own internal billing and team about this because it is very complex. The answer is that hospitals do this all the time. Think about any multidisciplinary team where the patient is seeing an oncologist and a surgeon and then
then they also have an APP involved in their care. Hospitals are typically not leaving money on the table when they're performing really expensive services like this. And so most practices do actually bill for the majority of things as long as those services are independent. So they're documenting that these services are different from one another and that they're following the rules and regulations that their payers require when following these services.
But it's that second piece. It's the rules, the regulations of what the payers require for both documentation, what codes they use, and the filling out of the forms when these services are all being kind of combined or bundled that is so nuanced and really not part of what we would expect typical clinicians to know. So know that these things are happening, know that they're legitimate, that whenever
ever taking care of the best patient requires this. That's what you should do. Just make sure you're having an informed conversation about it with your billing team. And then how does that work in terms of I often have grad students rotating through the practice I work at.
And so does this affect at all? Like, let's say, you know, at first they're shadowing and then they're like, all right, like do a little part. Maybe they start with carrier screening or something. And hopefully by the end of the rotation, they're doing full sessions and I'm sitting back and then just commenting at the end if there's anything that's missing. Is that a problem in terms of billing? Can I still bill for that time?
With the genetic counseling student being really the lead genetic counselor in that session, I'm obviously paying attention, taking notes and all of that and jumping in if needed. But, you know, hopefully it's not needed, right? Because we want our genetic counseling students to be like, yep, I'm running the show. So is that an issue? Such a great question, right? So many of us have students. It's like top of mind, especially because the language in the code says brain genetic counselor.
What I will say is that 96040 also said train genetic counselor. So if you were previously working and doing the same thing and your billing team allowed it, I'm not anticipating any changes. Absolutely. This is one of those conversations that you have to have with your compliance department to make sure that everything is smooth. But because this code is now modernized so that it's very similar to what you're doing or what our
colleagues are doing that use E&M codes like our physicians and APPs, we can pretty much expect that the rules that they follow for a fellow, so someone who's maybe a medical student is the best example, right? Medical students are not yet trained doctors.
whatever rules they're following, work for us too. Yeah, that's really helpful to know. And I think that also makes me think of genetic counseling assistants. So luckily in our field, this has become more and more, there's more positions available. A lot of people that have these big teams, I imagine you guys have GCAs involved. So what if say a GCA is calling the patient like that day, getting that outline family history that sometimes they do so that the genetic counselor has this kind of skeleton to work with and confirm some information.
Can we bill for the time that the GCA is doing that? Or is that, nope, that's going to be separate because they're not a provider in that sense? Yeah. So another really common question that we've been getting, we are really excited because for the first time in this code process, we were able to get GCAs valued as part of the code.
However, we cannot report them separately. And there's a really good reason for this. When you think about the E&M codes that physicians and APPs use, when it comes to their time, even if it's a physician and APP working together, their time is counted independently.
But if you think about the nurse who is performing vitals on the patient or another care team member that is considered staff, those individuals' time is not reported independently because it is assumed that that's going to be something regular that they're doing as part of every visit.
That is exactly how genetic counseling assistants got valued into this code. We assume that moving forward, many practices will be using GCAs and doing so in a relatively standardized way. Maybe they'll be having them room patients or having them help take parts of it.
So the AMA included that value as a fixed value in the code. And so there is value. You can take that. You can use this information because they released this in a statement to CMS to say, hey, this supports our need to have GCAs. But you won't report that time separately when you're documenting the code because it is baked into the time. It is assumed that it's being performed, but not reported separately.
Okay. So if the, say the GCA takes a half hour on the phone with a patient and then the genetic counselor meets with that patient for a half hour, we're not, are we billing for 60 minutes or 30 minutes?
30 minutes. 30 minutes. So we're not counting that towards the time. And from my understanding, it's similar to before, whereas a 30-minute time block, you're using the code. Is that the same? I also remember something about 16 minutes. So I've rushed my memory on this part. Yeah, no, absolutely. And before we tie up that last bit, I will also say, though, that there are a number of CPT codes that are meant for staff usage.
Okay, so it could be we're billing for something separate for that time. Exactly. So one of the most important phrases that we use is not reported separately when we talk about CPT codes. For example, say a genetic counselor also has a phlebotomy license. They wouldn't count 96041 for the time they're drawing blood.
Because there's a code for that. There's a code for drawing blood that hospitals use. So even if they can wear multiple hats as a genetic counselor, they're really only going to be using 96041 for the time that they're providing genetic counseling.
If you think about genetic counseling assistants, their staff is part of the healthcare team. So what they're performing is a task that's being regularly done over the phone for which there may be another code already available to staff. It's not that their time can necessarily go unreported. It's just that you may be using a different code for it. That's very helpful. Okay. Keeping it separate. That makes sense. I like the phlebotomy example too, because there are some genetic counselors that will draw blood. And yeah, that's not a genetic counseling task per se.
Exactly. And then Kira, what was the next part? 16 minutes. Yeah. What about the 16 minutes? And take me through if, let's say, I prep for a half hour, I meet with a patient for a half hour, how do I bill for that?
Yes. So for the time reporting increments, as soon as you hit 16 minutes of total time, we are now eligible to use the code. So that can be any combination. There is no 50% rule. So some people have heard that term, particularly from the evaluation and management codes where half of the time for reporting has to be directly spent with
the patient. This particular code 96041 is not in the evaluation management section of the code book. It's in its own, it's in the medicine section. And so there is no 50% rule. Any combination of time with a patient or time in preparation or documentation can count. However, one common question that we get is, well, could I use this code for a patient that no shows, but I spent more than 16 minutes of prep?
And the answer is no. The code does specify that an encounter with a patient has to happen. So there has to be person time to use 96041. But as long as you're meeting that 16 minute threshold. And then after that, in the codebook, there's a table to show you exactly when to roll over.
And I'm not going to say the specific minutes because during the process, we changed it so many times that my brain actually... That's totally fine. We'll throw the table in the show notes for people so they can just take a look at that. Yeah, definitely. Well, anything else as we close out? I mean, this is very, very helpful. I'm certainly going to send this to the billing person at my practice to be like, hey, this is what we're doing now. Any other final advice or thoughts for people just as, you know, January 1 is getting closer for us to be able to start using this code?
I'd love to hear from Colleen on how the payer efforts are going and if we had any good news.
So we are still working on contacting payers. The other thing the NSGC Board of Directors is currently doing is looking at third party, third parties who can who have expertise and contacts in this area. And so we're evaluating proposals and we'll be hiring a firm to assist us with this. And so I think, you know, we were filling in, we're totally redoing our government and payer relations and advocacy infrastructure, which I think is great. And it'll help meet and the
the needs of our growing community and also help continue to improve reimbursement for genetic counselors. So I'm really excited about that. I think my last kind of final advice would be it's okay if not everything goes right on January 1st. We actually anticipate not everything will go right on January 1st or January 2nd if you have the first off.
And that's okay. That's normal. It happens. It's not unique to our code. It's not, you know, this happens when I was talking to my own institution about it. They said, yeah, let's
let's touch base in March and we'll see where the pain points are. They said a lot of times, you know, things might get denied at first by the payers and the payers see like a massive amount of denials and then they're going to, that'll trigger them internally to go and look and make sure that they update everything. So this is going to be as much as we want to control it all, as much as we want to have it
perfect. It's not going to be perfect right away and it's okay. It will get better and it will improve. And I think when we think about the big picture, yes, there's going to be some bumps in the road, but long-term, this is going to be much better for our profession and much better for the patients we serve because that'll improve, this will help improve their access to us. So I think this will be really good. And we just ask for, you know,
you know, we're just going to have to breathe through this and get through those bumps initially. The other thing I would be remiss if I didn't mention is a huge thank you to ACMG who worked with us on this new code, as well as Brian, Matt Katz, the whole CPT work group that has been working tirelessly on this. Without their help, this wouldn't be possible. So from the NSGC Board of Directors, very grateful to ACMG and the CPT working group for all their work on this.
Yeah, yeah, definitely. And I think my last door handle question is, you know, patients right on the way out, they're like, oh, by the way, like, that's not actually my bio father or something, right? So as you said, Colleen, I think realistically, not everything is going to happen January 1, 2, 3, whatever, right? So if places are still using the old code, is that just not going to work? Or does it still work? Is there a grace period for people to be adopting and using this new code? Or do we not know?
The funny thing is it will work with the payers that haven't switched and it won't work with the payers that have switched. So it's really specific on that relationship. Wow. The best advice is to switch to the new code because that is the intended correct way to do it moving forward. And let the payers be in the wrong when they're denying it because that gives you a really good place to stand in and say, hey, this did update. The AMA and CMS have listed this as of 2025.
Awesome. Well, thank you for that. Really appreciate both of your time just being the busy month of December and everything. And thank you so much for all the presentations you've done over the past few months, just so that everybody is aware. And we're going to put a bunch of links in the show notes, especially NSGC's billing slash CPT resources, because there's a page with a lot of great stuff. I watched the webinars that you guys did live over the last couple months. And also I saw that it's going to be released.
clinical workflow considerations and a historical timeline of 96041. So I'm looking forward to that being added to that page, but that's in the show notes for people if you want to check that out and you just need a quick reference and not a half hour podcast episode. So thank you, Brian and Colleen. Really appreciate you coming on and breaking all this down for us. Thank you, Tara. Thank you.
For more information about today's episode, visit dnatoday.com, or you can also stream all 200 plus episodes of the show, including video versions of interviews recorded in 2021 or later. Any questions, episode ideas, guest pitches, or sponsor inquiries can be sent into info at dnatoday.com. Be sure to follow us on social media, especially so you don't miss a giveaway. We are at DNA Today Podcast on Twitter, Instagram, LinkedIn, Facebook, and more.
Please rate and review the podcast on Apple, Spotify, or wherever you listen. This truly helps us climb the charts and allow more genetic nerds like yourself to find the show.
Here's a bonus. If you do and send us a screenshot, I'll give you a shout out on the show. DNA Today is created, hosted, and produced by myself, Kira Deneen. Our team includes communications lead, Corinne Merlino, video lead, Amanda Andreoli, outreach intern, Sonia Tanaykar, social media intern, Kajal Patel, and graphic designer, Ashlyn Anokian. Thanks for listening and join us next time to discover new advances in the world of genetics. The genes of you and me. The genes of you.
And they're all made of DNA We're all made of the same chemical DNA, DNA
Looking to jumpstart your career as a genetic assistant? These essential roles involve patient communication, data management, genetic testing coordination, and admin tasks, making proper training a must. The Genetic Assistant Online Training Program at Johns Hopkins University School of Medicine is a top choice. DNA Today listeners rave about how this course boosted their genetic counseling skills and prepared them for grad school.
The spring cohort starts soon on January 27th, so apply now before it's too late. The program includes two 10-week instructor-led courses. Armed with a basic science background, you'll earn a certificate from the Johns Hopkins School of Medicine upon completion. You'll also gain practical skills and insights from leading instructors that will give you a competitive edge in genetic counseling and related fields.
Learn more at dnapodcast.com slash sponsors or simply search Genetic Assistant Online Training Program, Johns Hopkins.
When it comes to your health, knowledge is power. I've always believed that the more we understand about our bodies, the better decisions we can make, whether it's about the food we eat, the exercise we choose, or how we plan for the future. But traditional healthcare often feels reactive and not proactive. That's why I'm so excited about 23andMe Plus Total Health, a longevity platform that puts you in the driver's seat of your health journey.
Again,
Again, that's 23andMe.com slash DNA Today. You can also find this link at DNAToday.com. Take charge of your future health with 23andMe Plus Total Health because your health deserves a personalized approach.