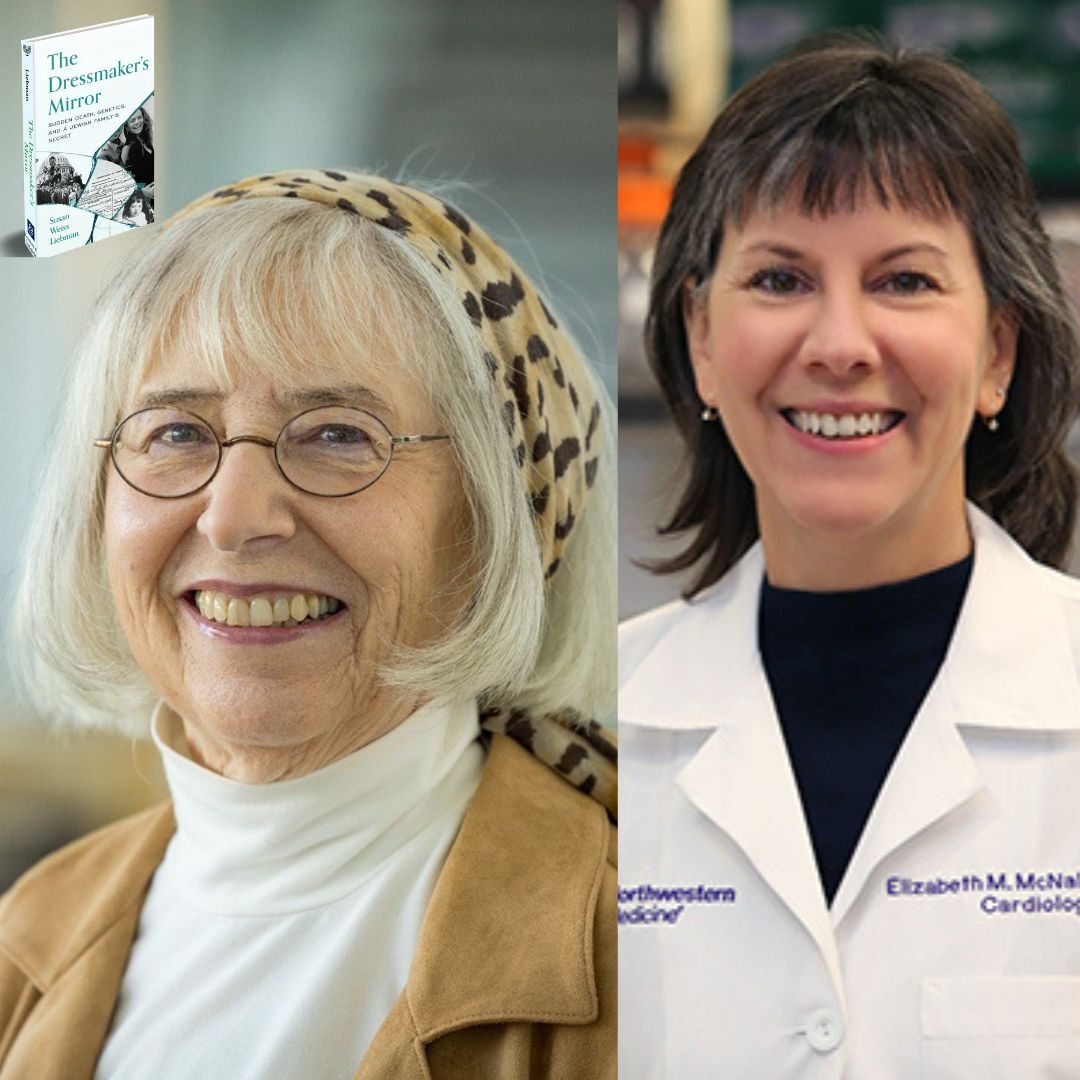
#315 Preventing Sudden Cardiac Death via Genetics with Drs. Liebman & McNally
DNA Today: A Genetics Podcast
Deep Dive
What tragic event in Dr. Liebman's family led her to write 'The Dressmaker's Mirror' and advocate for genetic testing?
In 2008, Dr. Liebman's 36-year-old niece, who was six months pregnant, suddenly collapsed and died from undiagnosed dilated cardiomyopathy. This event, combined with her sister's earlier diagnosis of the same condition, motivated Dr. Liebman to write the book and advocate for genetic testing.
Why is family history crucial in identifying genetic heart conditions?
Family history is crucial because it can provide early warning signs and help identify genetic mutations that may cause heart conditions. In Dr. Liebman's case, her niece's sudden death and her sister's diagnosis of dilated cardiomyopathy suggested a genetic link, which led to further testing and identification of the FLNC mutation.
What significant discovery did Dr. McNally's team make regarding Dr. Liebman's family?
Dr. McNally's team identified a mutation in the FLNC gene, which was responsible for the dilated cardiomyopathy in Dr. Liebman's family. This mutation was not initially recognized as a cardiomyopathy gene but has since been confirmed and added to genetic testing panels.
Why is genetic testing for cardiomyopathy underutilized, and what are the barriers to increasing its use?
Genetic testing for cardiomyopathy is underutilized due to a lack of trained professionals, insufficient awareness among healthcare providers, and concerns about the cost and complexity of testing. Only 1% of cardiomyopathy cases are referred for genetic testing, despite mutations causing nearly 50% of cases.
What are the next steps after identifying a genetic mutation in a family member with cardiomyopathy?
After identifying a genetic mutation, the next steps include monitoring with a wearable heart monitor, conducting stress tests, and imaging to check for heart scarring. If necessary, patients may be recommended for a pacemaker or defibrillator to prevent sudden cardiac death.
What is the significance of the FLNC mutation in Ashkenazi Jews, and what are the implications for population screening?
The FLNC mutation is more common in Ashkenazi Jews, with one in 800 individuals carrying it. This suggests that population screening for this mutation in Ashkenazi Jews could be beneficial, as it can lead to early detection and preventive care. However, there are debates about the feasibility and necessity of widespread population screening.
What are the future prospects for gene therapy in treating cardiomyopathy?
Gene therapy for cardiomyopathy is an active area of research. Companies are developing treatments for genes like MYBPC3, LAMP2, and PKP2. The challenge is timing the delivery of the therapy to patients who are sick enough to benefit but not too far gone for rescue. Early-stage and preventive applications are also being explored.
Shownotes Transcript
Looking to jumpstart your career as a genetic assistant? These essential roles involve patient communication, data management, genetic testing coordination, and admin tasks, making proper training a must. The Genetic Assistant Online Training Program at Johns Hopkins University School of Medicine is a top choice. DNA Today listeners rave about how this course boosted their genetic counseling skills and prepared them for grad school.
The spring cohort starts soon on January 27th, so apply now before it's too late. The program includes two 10-week instructor-led courses. Armed with a basic science background, you'll earn a certificate from the Johns Hopkins School of Medicine upon completion. You'll also gain practical skills and insights from leading instructors that will give you a competitive edge in genetic counseling and related fields.
Learn more at dnapodcast.com slash sponsors or simply search Genetic Assistant Online Training Program Johns Hopkins.
When it comes to your health, knowledge is power. I've always believed that the more we understand about our bodies, the better decisions we can make, whether it's about the food we eat, the exercise we choose, or how we plan for the future. But traditional healthcare often feels reactive and not proactive. That's why I'm so excited about 23andMe Plus Total Health, a longevity platform that puts you in the driver's seat of your health journey.
With 23andMe plus Total Health, you get advanced genetic screening, giving you insights into your potential future risks, and comprehensive blood testing throughout the year to track how your health is changing. It's a level of personalized care that goes far beyond the one-size-fits-all healthcare system that unfortunately we're used to. Advocate for your health today. Go to 23andMe.com slash DNA Today to receive 10% off your Total Health membership.
Again, that's 23andMe.com slash DNA Today. You can also find this link at DNAToday.com. Take charge of your future health with 23andMe Plus Total Health because your health deserves a personalized approach. How is it that we find ourselves surrounded by such complexity, such elegance? The genes of you and me. The genes of you.
They're all made of DNA We're all made of the same chemical DNA
Hi, you're listening to DNA Today, a multi-award winning podcast and radio show where we discover new advances in the world of genetics. From genetic technology like CRISPR to rare diseases to new research. For over a decade, DNA Today has brought you the voices of leaders in genetics in over 200 episodes. For the past three years, DNA Today has won the People's Choice Best Science and Medicine Podcast Award. I'm Kira Dineen. I'm a certified genetic counselor and your host. ♪
In this episode, we're chatting with two experts in genetics, as we do on most episodes. Dr. Susan Liebman is a pioneering molecular geneticist who has dedicated her career to understanding prions and protein-misfolding diseases such as ALS and Alzheimer's. Dr. Liebman has been instrumental in using yeast as a model organism to uncover the mechanisms behind these complex diseases. Dr. Susan Liebman is a pioneering molecular geneticist who has dedicated her career to understanding prions and protein-misfolding diseases such as ALS and Alzheimer's.
She's also an author. Her new book, The Dressmaker's Mirror, Sudden Death, Genetics, and a Jewish Family Secret is a deeply personal account that intertwines the discovery of a previously unknown heart disease gene with the story of her family's journey through love, loss, and resilience. She also has some pretty big name people that have endorsed the book. Dr. Siddhartha Mukherjee is one that's a pretty big name, but you know, we'll get to all that. Our
Our second guest is Dr. Elizabeth McNally, a distinguished cardiologist and geneticist who serves as the director of the Center for Genetic Medicine at Northwestern University. McNally's research focuses on cardiovascular genetics and neuromuscular diseases, as she has been at the forefront of integrating genetic information into patient care, which is a big part of our conversation today. And
How these two amazing guests connect is that Dr. McNally's collaboration with Dr. Liebman's family led to the identification of a genetic mutation responsible for sudden death in Dr. Liebman's family. And this discovery has profound implications for genetic medicine and preventative medicine care. So in this conversation, we're delving into groundbreaking research, exploring the emotional and ethical
ethical complexities of genetic testing and discussing the future genetic screening and personalized medicine. So I think we have a lot to cover here, guys. Thank you so much, Beth and Sue, for coming on the show. I really appreciate being able to hear from both you in this episode.
Great to be here. Yes, thank you for having us. So as we said, I think we'll go with Sue and Beth as we record here. And so Sue, your book, The Dressmaker's Mirror, is inspired by many tragedies in your family. Can you share what your family has experienced that led to your advocacy and motivations to ultimately write this book and capture your family's experience and raise awareness?
Well, the big event was in November 16th, 2008, when my newly married six month pregnant 36 year old niece in the prime of life was at a restaurant with her husband to celebrate his 37th birthday. And she suddenly collapsed with no warning whatsoever.
They were in downtown Brooklyn. There were ambulances there within minutes. She was in the hospital within minutes, but they were never able to restart her heart. She died instantly and her unborn baby died that day as well. There was no warning to us or to her, but there was a warning. She had told her doctor that she was out of breath. She had told her doctor that she had a cough she couldn't get rid of.
And the doctor said, well, you know, you teach third grade, you're catching a cough from your kids, and everybody who's six months pregnant gets out of breath. So those warnings were not seen. Ten years earlier, before Karen's death, my sister, in her mid-50s, had a long relapse.
road also to diagnosis. She had a cough. She also was a teacher. They said it was pneumonia. They said it was bronchitis. Finally, her daughter-in-law, who was a physician, came and looked at her and she gave one look at her and said, you know, I think you're in heart failure. Diane went to a cardiologist. It was confirmed that she had dilated cardiomyopathy. But because of the lack of family history and no other environmental factors, she wasn't
on drugs or anything, they said that this was probably due to a virus. This was the long-term effects of a virus. So when Karen died, the New York City coroner's office actually removed her heart and sent it away for further analysis because they found nothing from the straightforward autopsy. And the result that came back shocked the family. The result was that she had dilated cardiomyopathy.
So it was pretty obvious that the mutation, that a virus was not the cause of my sister's illness, that rather it was likely a mutation. And I became terrified for my family. And also I had a daughter who was then pregnant as well.
So the question was, was this mutation new to my sister? So I was free of it. Or did it come from my parents or further back? And were we all at risk? That's the major impetus for writing the book and telling the story. And such a, obviously, tragedy in your family that not only losing your niece so young, but also she was pregnant, she was married. It's like this new phase of her life was just starting to pick up.
And it's really heartbreaking that in many of these cases, as we'll talk about today, the first sign of the condition is sudden death. And there often isn't red flags ahead of time that we can catch it before that.
But as you mentioned, Sue, you didn't have any symptoms. You kind of learned about this. Okay, my niece had this condition and my sister has the same condition. There most likely is some kind of genetic factor behind it. So with all of those moving pieces, how did you become Dr. McNally's patient then? How does that work when you yourselves don't have symptoms? Dr. Sue
So I was very concerned about this. I talked about it all the time. And one of the places I talked about it was at the yeast genetics club in Chicago, since I'm a yeast geneticist and there's a bunch of geneticists there. And lo and behold, lots of them knew Dr. McNally and they knew her husband, Steve Krohn, because he was doing research on using yeast as a model organism, just like the rest of us.
And several of them said, she's the person to see. She's the top person in genetic cardiology. Steve Meredith, in particular, gave me your name, Beth. And so I made an appointment and I became her patient. That was serendipity and very lucky for me. And I think that's right, which is family history is still a very powerful tool to use and thinking about your own health. And so
a lot of times people don't share enough information about family history, which is I think a big point of Sue's book and take some digging sometimes to get to it. But when you have one person in the family that has cardiomyopathy, you know, that alone is enough to alert some things. But here we had a second case in the family and we had a sudden death associated with it. So those then, you know, raise it up
for more, 10 more levels of like why you should get care because the risk is as high as 50% that you're going to have the same thing. And of course, it's as low as 0%. And genetics can sometimes help us solve that problem. Sometimes it doesn't. There's still lots of cases that we don't solve, but many that we do. And when we don't get a genetic test, that's still a recommendation in all our guidelines in cardiology, which is that if you have a relative who has cardiomyopathy, you should get screened for it.
When it comes to family history, being a genetic counselor myself, I think one of the areas of genetics where family history is the most important may be cardiology because in a lot of other areas like cancer, that's also very important. But I think with cardiology and looking at any cardiovascular conditions,
Looking at that family history, it may be the only sign if there is a sudden death in the family. I know when I'm taking family history, OK, I got to refer this to someone that works in cardiac genetics because I may be the only one that picks up on this. Right. And so I think that's really important. And so in your family, through this process of your niece, your sister, it's like you start exploring more. Right.
And you uncovered a family secret that had been a secret for probably 100 years by the time you learned about it. Can you tell us a little bit about who would have been your uncle and how if you had had that information earlier, how things may have been different? So when I was six years old, I was looking at family pictures and I saw this picture of this kid. And I said to my dad, who's this? And he said, oh, that's my brother. I said,
what? You know, it doesn't look like Uncle Cyrus. And he told me that he died when he was four. And his mother, his mother was a dressmaker. She worked at home sewing. Big, heavy mirrors fell on the kid and killed him. And this was horrifying to me. My
It stayed with me my whole life, this terrible story. My uncle, the living uncle, told it to his family. It stayed with them. This was family lore for over 100 years. I'm sure my uncle and my father believed this story. My father was two when this happened.
And as I was writing the book, almost finished with the book, I decided to just, you know, check the death certificate. It was actually some deal about when did this baby die? Was he older or younger? And so I was checking it out. And when I looked at the cause of death, there wasn't any injuries and there wasn't any accident. And he died of heart failure.
And so four years old, which is four years old, very young. We don't I don't know, Dr. McNally, can you weigh in for a moment? Is that something that is that we often see in families that have cardiac issues? Like to me, four years old is like that really stands out.
So we do, and I actually work pretty closely with our colleagues across the street at the Children's Hospital because we do. When they're very young, certainly in the first year of life, often those are de novo mutations, not surprisingly. That makes a lot of sense. And there's particular ones that show up. Random change, not inherited. Yep. Random change that shows up, brand new mutation in that child. Yeah.
The other possibility and the one I think I had mentioned to Sue is that it could very well have been that he had the primary mutation but then had a second hit that made it show up so early in life. Because typically with filament C, we don't think of it as being
that early in life. And now that we can do complete genomes, we're starting to get some better tools for integrating second hits, which by the way, don't have to be so rare. It can be even a lower frequency, but not super rare variant that can be the second hit because you're on top of what is already a mutation. So that's where we've still got to go with genetics.
Yeah, a lot of complexities that there can't be two mutations that just has that compound risk to it. And Sue, to go back to what you're saying, because I cut you off a little bit, but I just wanted to kind of capture Dr. McNally's perspective on that.
So you're learning about this. I didn't realize until this moment that it was towards the end of the book. I thought maybe you knew this was what you were outlining. Towards the end of my writing. Sorry, sorry, towards the end of my writing. And I do mention it. I give the answer at the end of the book. So we're giving a little away here. Spoiler alert. But that's the way I found it. The whole time, I had no idea until the very end.
Certainly, if we had, and I found that there's articles about it in the newspaper. And what happened was the family moved away. They moved right away. They left Carbondale and they moved to a different city where people didn't know about it. And they came up with this tale. If we had known a diagnosis of heart failure, I do think that when my sister came down with heart failure, or all those things that looked like heart failure, they would have diagnosed her sooner.
And if she had had a diagnosis at that point, I do think that there would have been more of a chance that Karen's doctor wouldn't have said, this is because you're pregnant and you caught a flu. They would perhaps have checked her and she might have been saved. But yeah. And that's such hard reality of the situation. I did want to point out here that, um,
There were other things in my family that we didn't know about. And that's because people die of a lot of different things early. We had people dying of diphtheria, of cancer. And so they may have developed this, but we wouldn't know about it. And also, of course, people can have the mutation and not ever present. Family history is helpful, but as Dr. McNally was saying,
We go ahead with genetic testing sometimes without family history. This really plays a role in terms of doing genetic testing, because at the time, the gene that was found to house the mutation for your family, it wasn't on panels. It wasn't really known at that time. Dr. McNally, if you don't mind kind of sharing a bit, like, how did that process go? Because
To me, this is not something that even a lot of people in genetics kind of know how this works in terms of you have an individual that has passed away. How do we then start doing cascade testing? Like, what are we looking at? How do we end up being able to use that tissue? There's a lot of
nuances here that is very different than when we have a living patient. We knew about filament C actually from the skeletal muscle field first. And as I mentioned, skeletal muscle genetics and now treatments have moved on a little more quickly than some of the cardiac genetics and treatments. And I always view that as sort of the window of what may come next for us in cardiac genetics.
But we knew about filament C being associated with skeletal myopathy. And if you looked and read those papers, it was also clear that many of the older members of the family, and I don't mean very old, but not children, also developed cardiomyopathy and arrhythmias very frequently as well. So we published a paper in 2014
which was using whole genome sequencing to try to demonstrate whether you could identify cardiomyopathy mutations using whole genome sequencing. At the time, panels started out just a few genes and were growing a little bit bigger and bigger and bigger. And it was just getting frustrating. So, you know, being a little bit ahead of the curve, we were like, let's just see, can whole genome work? And we laugh now, but I had a wonderful Sarnoff fellow in the lab for the year who was doing this. And we were, she was doing it.
manually looking through this genome because we just didn't have the tools. I mean, she probably started this, I think 2012. It took a while to be able to do it. But in that first paper where we published Jessie Goldeson, she's a heart failure doctor now, wonderful doctor.
published this paper where she showed she could find these mutations. And in among the families we described in that paper was actually Sue's family, where we had found this filament C. And it was a little tricky because it was not accepted as a cardiomyopathy gene mutation at the time, but we had enough evidence that we thought that's what it was. And we borrowed from the skeletal muscle literature and what was there. We made the case, the reviewers picked on us about it, of course, but we pushed back. And so that actually is the first
pure cardiomyopathy report there. But around the time we put that out, there were a bunch of other people. I remember having a conversation with Matt Taylor, who's a wonderful geneticist in Colorado. And he's saying, yeah, we got these filament families, but sometimes we find second hits. And so we don't know what to do with it. And I was like, you just need to publish it.
publish it, publish it. The more we get it out there, then it starts to become more accepted that that's what this is. And so by the time Sue reached out to me to contact me again a couple of years later, that's when there had been this second and third and fourth reports. And so we started to have a lot more confidence that that was what was going on. We had to push to get, um,
some of the companies to get it on their panel. They had the gene on their skeletal muscle panels, but they refused to put it on their cardiac panels. And we kept saying, look, here's all these papers. You've got to test this also. And now I think it is, if you look at our paper that we published in 2022, it's like- Which we'll link in the show notes for people that want to read it. Fourth or fifth most common gene now for
for cardiomyopathy. So just going from pushing it, hey, please, these genetic testing companies include it on the panel. We want this to be included when someone orders a cardiac panel. They're like, I don't know what's going on. Let's start here.
And then to jump up to be, that's how frequent mutations are coming up when people are ordering this panel, like if a mutation is found. Yeah. And the trickiness with filament C is that the cardiomyopathy can be a bit buried. You can see dilated, but maybe not the most dilated heart and a little bit toward the
toward hypertrophic or even restrictive, but not the most prominent. But there's a very prominent ventricular arrhythmia signature with filament C. So it's absolutely one of those genes that when we get that back, we use different parameters now for monitoring patients much more closely who carry this and then recommending device earlier than we would normally do it otherwise. So it's a clear gene that we act on because it has this prominent arrhythmia component with it.
And to me, that's what's so important. And what, again, is another, I guess, special aspect in cardiac genetics is a lot of times when we identify there is a pathogenic variant mutation that's elevating someone's risk for some kind of cardiac problem, a cardiac event.
Oftentimes there is prevention. We don't necessarily have that in every area of genetics, but cardiac is one where it is so important and lifesaving in most cases. When we do have someone that's identified and keep going with the genetic change found in Susan's family. All right, we have this diagnosis in someone.
What are those next steps in terms of preventing? Like, is it standard to say, okay, this person needs a pacemaker. This person needs to do a stress test. How does this work? What is the gene? Genetic information is one piece of an algorithm that we're using. And so the algorithm is.
you're probably gonna have somebody wear a monitor first and foremost. And now the other thing that's happened is we've got, since 2018, we now use these patch monitors that we put on the skin, doesn't have all the wires and things sticking out, just sits right here. You can wear it for up to 14 days.
You send it back to us and we get 14 days of really high quality monitoring. We also have lots of people wearing these things, which are really just good for AFib, but can sometimes detect some other things. I have had people send me VT on their watch. So this is a podcast. She held up a watch.
Yeah, sorry. We held up the watch. I have an Apple watch on. We can still see ventricular tachycardia on that. So that's important. So monitoring first and foremost, patients being knowledgeable about their symptoms. Do you have palpitations? Do you feel like you're going to faint? Have you fainted? Those are really important. Putting people on a stress test, seeing whether that triggers abnormal rhythms, and then imaging.
And for us, that's MRI imaging, because if we see evidence of scarring in the heart, that's like, you know, you're adding up points for all of these. Does it trigger non-sustained BT? Do you see scar on the heart? And do you have a gene mutation? All of those things are going to add up together for who gets a device. But the gene alone is certainly just one piece of the puzzle.
So an important part of the workup, but we need to have the rest of it. So once this mutation was identified in your family, Sue, were you then on this track of, okay, we have to get family members tested? Like who was the next person? Was it yourself? Yeah.
Yes. So Beth and Lisa from her office wrote a dear family letter, which I sent out to family members. But I had to, some I knew, but there was a lot of family members I didn't know. So I became an amateur genealogist. I really spent two years finding people and sending out this letter. And the letter was,
was a great letter, but I had, I learned that I was going to put people off with that letter. I had to tell them, hi, I'm your cousin. You, I, I'm related to so-and-so's grandma was my sister's, you know, and then they would talk to me more if they didn't know me, if they knew me and if they knew Karen.
Then they wanted to know this information right away. So that was a whole new world learning how to reach people right now. I do want to mention this, this organization called Connect My Variant. Do you know that place? Yes, they've actually come on the show before. I know you do, but I don't know if Dr. McNally knows them. They can help you find information.
relatives. So they want you to put in your variant and then they will use genealogists, professional genealogists to help you to find them. So that's a big thing. And of course, at the time, I didn't know if it was from my mother's side of the family or my father's side of the family. And that's because even now that we knew the gene, we didn't have my mother or father's DNA.
And so I did want to mention that it's now possible to save your DNA. You could, of course, get your DNA secret, but there are various companies. One of them is SecuriGene that will bank your DNA so that if your children or grandchildren want to figure out something about the family history, they can do that.
And the last thing I wanted to mention was just amusing being a yeast geneticist, that when I heard about what the gene was two years after the paper was published, I, of course, started searching for it. And the first hit I had was published at almost the same time as Dr. McNally's paper. It was published by a guy named Fritz Roth, whose father, John Roth, was a yeast geneticist.
And it all comes back to yeast. The patient who had this exact mutation had the exact same ejection factor as my sister, but had checked off. Do not bother me. Don't call me. So there was no way to contact him or his family to tell them anything about it. Yeah. So it becomes a challenge sometimes when it's like you want to reach out, but it's not always an option or even just finding those, those people, as you said, to be able to do that testing. And,
I think a big part of this too is, yeah, being able to identify who is at risk and do that testing and having them understand all this. Yes. And what I also learned was I had to begin with, and there's something you can do. Yeah, it's actionable. You can start with, you know, we can help prevent a problem, not that there is a problem and you might die. That doesn't get them to read the rest of the letter and then they're very angry with you. The other thing that was interesting was
Two years later, another paper came out, a lot of authors. One of the co-authors was Dr. Michael Arad, and he had two patients who had the exact same mutation as in my family. And I corresponded with him by email, and he said to me, hey, by the way, looking at my name, are you an Ashkenazi Jew? Because my two patients are Ashkenazi Jews. And then I looked up in the
irritable bowel, no, I think that's the name of it, irritable bowel database was one of the best DNA databases at the time. And one in 800 Ashkenazis in that database, but nobody else had that mutation. So it was a founder mutation then? It was a founder. So it wasn't new to my sister. The important thing to my family was it wasn't new to my sister.
I was at risk. Somebody in my family, my mother and my father had it. And so finding all these relatives working on that tree was valuable. And that begs the question, too, of there's been talk a lot over the years, just in general, of doing population-based screening and testing for these types of conditions where we know certain populations are at an elevated risk.
to be a carrier basically of these genetic changes and then have the risks that go with it
Do we think that this should be offered for people of recent or enough Ashkenazi Jewish descent because they do have a risk to this? I don't know if either of you want to weigh in on that just because it is one in 800. Like that's to me, that's kind of high. But actually, in the general population, it's even higher to have any mutation that causes myopathy. Right. So if we're going to test Ashkenazi Jews for this one, we should test everybody for all of them since now we can sequence everything. Right.
And there's a lot of debate as to whether to do testing. So it actually was very confusing to me, these expectations
You don't want to test unless you've got a good, unless you can help people. Obviously the American College of Medical Genomics has looked into this and they've picked out 81 genes. I think there's about 38 of them that affect the heart that if you find imitation and then there's something you can do about it. But what they suggest is very weird to patients. And that is
If you find a mutation in one of those genes by accident, you're testing them for cancer, but you come across this heart disease gene, you should tell your patient. But you shouldn't screen for it. We shouldn't have screening. And I try to understand this confusion. So the best I can understand is, and maybe Dr. McNally can weigh in on it, is they say, well, we don't have enough doctors and they're not well-trained enough that if we start doing it for everybody, we're going to go nuts.
And the second concern they have is that sometimes a mutation that is pathogenic in one family and one ethnicity will not be so in another ethnicity or in another family. And it's particularly a problem for rare mutations. But it appears that, you know, I don't know if it was your study or someone else's study, Beth, but that when they went ahead and looked at random at people,
One in six people that didn't have any symptom and didn't have any family history came up with a mutation that could be treated. In my view, we really have to solve the problems. And I'd like to see genetic screening. And maybe the place to start, too, is just having people that are at risk for these different cardiomyopathies to get them tested before we start trying to screen populations in general for these because, again,
And I think I read this in the book, although mutations cause nearly 50% of cardiomyopathy cases, only 1% are referred for genetic testing. Dr. McNally, from your perspective, how do we at least try to tackle this first? Because that is alarming. A lot more people need to be offered genetic testing. And I'm biased as a genetic counselor that I think everybody should be offered it, but especially in this case.
So you have a workforce problem with cardiac genetics. I'm happy to say it is slowly improving.
the real issue is that people are not trained how to do this. We don't have enough counselors. I mean, we've had a very successful model over many years of working with counselors and having them fully integrated into our cardiac practice, but it's still a battle to try to explain like, why do we need a genetic counselor in cardiology? Well, we need it for this following reasons, because we have a lot of patients with genetic disease, whether we want to acknowledge it or not.
And that's, I think with therapies coming, that's going to begin to change things. But we still are woefully behind in our workforce education in terms of knowing. Now, the good side of it is genetic testing has worked its way into a number of the cardiac guidelines right now. So our arrhythmia colleagues, the electrophysiologists who manage a lot of these patients, it's in their guidelines. It's in the heart failure guidelines.
We do see it now in a number of places. So we are seeing this uptick of people understanding I have to do that. I have to think about how to do testing. But we still have a lot of docs that just don't know how to get the testing. We've done a lot of work on this in our group and other groups have worked on it as well. Their biggest complaints are I don't know how to order the test. I don't know what test to order. I don't know how to read the report when the report comes to me.
Those are like their issues. And those are big issues that we have to figure out how to solve. So we've been working on it. We've developed some educational models. We've worked with the Jackson laboratories. We've put those models up. American heart association is big on it right now. They're trying to develop some things, but again, our modules are free there at the Jackson labs and you'd,
You can just sign on and do them. You can get CME and CEU credits for doing it as well. But we think this is probably important. We're talking a little bit among the group of places that do this well about should we develop a formalized training program or a certification process for those cardiologists who want to learn how to do it.
But we are seeing progress. It's just more slowly than I would like to see. Where we've seen probably the most uptake of genetic testing is for hypertrophic cardiomyopathy. And I think because now there are treatments really directed at hypertrophic cardiomyopathy, that that's leading to more genetic testing. The genetic testing is not required for the treatment. The diagnosis is required. But it's...
It does make people think more about genetic disease. So far and away, I think hypertrophic gets the most testing. But for arrhythmia syndromes and the overlap of arrhythmias and cardiomyopathy, we think that's incredibly helpful, incredibly helpful to family members and can provide so much clarity for families to know what their diagnosis is and how to be managed properly.
And how do we manage? That's what's so important, because at the end, like, that's why we're doing all of this. And you mentioned different new aspects within treatment. And I think gene therapy is certainly one of them there. It's just been a lot more in the headlines recently. I think I look at, um,
Sickle cell in terms of being there's a CRISPR FDA approved treatment now. We had Victoria Gray on earlier in the year and talked about her being the first person that this was used on and successful in her case. What is on the horizon in terms of in this cardiac genetic space? And I don't know, how how do you see this first being used? Because in the case of sickle cell,
It's a little bit more straightforward because we can take out the bone marrow, as I've said, kind of crisper it up, put it back in. We can't take someone's heart out and crisper it up and put it back in. So this is there's a bit more of a hurdle there, I think, when it comes to gene therapy, when we're looking at things that are not blood related. What are your thoughts on, you know, the future here as we wrap up?
So the ones that people are working on right now in terms of target genes and conditions, and I had some conflict here because I talked to most of these companies because they asked me my opinion about them. And I'm always happy to share my opinion. So myosin binding protein C3.
turns out it fits within and it's what fits within the AAV vector. And is there evidence for loss of function of that gene as a contributing feature, so that putting more back is likely to correct the problem. So that's MYBPC3 for hypertrophic cardiomyopathy, Dannen disease, which is LAMP2. And so they've already treated a good number of patients with that. That's
a company taking that forward. PKP2 is on the horizon for arrhythmogenic cardiomyopathy, and several other ones are being looked at. But the point is the genetics has to line up so that it's partial loss of function and that there's evidence that restoring that function is likely to improve the situation. The hard part is figuring out what's the timing
of that gene delivery because right now with our current regulatory system, you need to do something that makes the patient better, which means they need to actually be sick. They need to have symptoms and be sick, and then you have to show that you make that better. And that's a little bit tricky because
You want a person that's experiencing some symptoms so that you can see you've made them better, but you also don't want a heart that's so far gone that it can't be rescued. So there's a lot of interest in it right now, several companies moving forward with it. And I'm hoping most of this will just pave the path for what will become even better therapies as we move forward that can be applied
late stage disease to help rescue some of that, or even when it gets safe enough to do even early stage disease so that we can really think preventively. But we've got some work to do. Yeah, it's exciting, but it is tough that you have to be sick, but not too sick.
Susan, anything else to close out the show? Yeah, I wanted to go back to the nice description of educating physicians, but we do have genetic counselors. And sometimes just telling the doctor, you don't have to know this, the genetic counselor is going to take care of it, will encourage them to move forward. And the other thing is, first of all, they still think it costs thousands of dollars. It's impossible to get them to understand that
It can cost a hundred or maybe no more than 250 maximum out of pocket. And so that you don't have to be afraid to order that for your patient. And the other thing from a patient point of view, many people, especially males, it seems reject the idea of genetic testing. They're frightened of it. They think it's going to change their life. They think it's going to make them have to go into, first of all, they might not be able to solve it. And if they can solve it, they're going to have to get tests. They might have to get an implanted defibrillator and they don't realize that
You're still going to have the mutation, even if you even if you put your head in the sand and having. And that was part of the book is to show the terrible tragedies are so much worse than having to go to the doctor twice a year, having a 36 year old daughter drop dead.
So I encourage people to realize that it's no worse than knowing you have high blood pressure or you have high cholesterol and there's something you have to do. And you have to, yes, get a blood test periodically and change your diet. There are things you're going to have to do. You might have to take a pill. You might have to get an implanted defibrillator, but you might live and your grandchildren might live. Right.
that that's just so important, that aspect that, you know, we're talking about life and death here. So it's really important to be able to do that. It's actionable. And that's not always the case for everything. You know, a lot of like neurodegenerative conditions, it can be scary to learn that because there's nothing to do right now for some of those conditions. But cardiac
so different. It's just, it's really empowering. And I definitely second what you said, Susan, just about, you know, pass along to genetic counselors. We're happy to get those cases. I don't work in cardiac, but you know, in the prenatal sector, when I get an OB, this is, I don't get this result. Can you handle this? Yeah, I would love to. So I think that's a big part. And I know we gave a shout out to Lisa earlier, who was the genetic counselor that was involved with your family, but thank you both so much. This has been just really informative and inspiring.
so important for people to understand. And it's also just exciting that cardiac genetics is growing so much in the past five years. We've really seen it. I feel like from my view of not being in the field of really exploding, a lot more people in genetics are working in this area and it's really promising and saving lives. So thank you both so much for coming on. I appreciate it. Thank you. Thank you so much, Kira, for what you're doing. And of course, Beth, for
changing my life. That's the other thing. If you find out you don't have a mutation, that's just, you know, you already know there's a risk in your family. Then there's relief. There's this tremendous relief. Yeah. And I should say, of course, you guys got to go check out the book, Dressmakers Mirror. So we're going to link to all, everything we talked about. I've been taking good notes in the show notes. So thanks guys for tuning in.
For more information about today's episode, visit dnatoday.com, or you can also stream all 200 plus episodes of the show, including video versions of interviews recorded in 2021 or later. Any questions, episode ideas, guest pitches, or sponsor inquiries can be sent into info at dnatoday.com. Be sure to follow us on social media, especially so you don't miss a giveaway. We are at DNA Today Podcast on Twitter, Instagram, LinkedIn, Facebook, and more.
Please rate and review the podcast on Apple, Spotify, or wherever you listen. This truly helps us climb the charts and allow more genetic nerds like yourself to find the show.
Here's a bonus. If you do and send us a screenshot, I'll give you a shout out on the show. DNA Today is created, hosted, and produced by myself, Kira Deneen. Our team includes communications lead, Corinne Merlino, video lead, Amanda Andreoli, outreach intern, Sonia Tanaykar, social media intern, Kajal Patel, and graphic designer, Ashlyn Anokian. Thanks for listening and join us next time to discover new advances in the world of genetics. The genes of you and me. The genes of you.
And they're all made of DNA We're all made of the same chemical DNA Made of DNA
Looking to jumpstart your career as a genetic assistant? These essential roles involve patient communication, data management, genetic testing coordination, and admin tasks, making proper training a must. The Genetic Assistant Online Training Program at Johns Hopkins University School of Medicine is a top choice. DNA Today listeners rave about how this course boosted their genetic counseling skills and prepared them for grad school.
The spring cohort starts soon on January 27th, so apply now before it's too late. The program includes two 10-week instructor-led courses. Armed with a basic science background, you'll earn a certificate from the Johns Hopkins School of Medicine upon completion. You'll also gain practical skills and insights from leading instructors that will give you a competitive edge in genetic counseling and related fields.
Learn more at dnapodcast.com slash sponsors or simply search Genetic Assistant Online Training Program Johns Hopkins.
When it comes to your health, knowledge is power. I've always believed that the more we understand about our bodies, the better decisions we can make, whether it's about the food we eat, the exercise we choose, or how we plan for the future. But traditional health care often feels reactive and not proactive. That's why I'm so excited about 23andMe Plus Total Health, a longevity platform that puts you in the driver's seat of your health journey.
With 23andMe plus Total Health, you get advanced genetic screening, giving you insights into your potential future risks, and comprehensive blood testing throughout the year to track how your health is changing. It's a level of personalized care that goes far beyond the one-size-fits-all healthcare system that unfortunately we're used to. Advocate for your health today. Go to 23andMe.com slash DNA Today to receive 10% off your Total Health membership.
Again, that's 23andMe.com slash DNA Today. You can also find this link at DNAToday.com. Take charge of your future health with 23andMe Plus Total Health because your health deserves a personalized approach.